The Brain
The brain of the infant is not mature to begin with. In a newborn baby, only the brainstem has all its functions firmly established, while the other parts are still developing their uses. Before an individual is able to bring into play all of her brain, the nets between the nerve cells of the brain must develop through the growth of branches from the nerve cells, and the nerve fibres must develop an insulating sheath of myelin. This maturing of the brain will take place all throughout childhood; however it is the very first year after birth that is the most crucial period for laying the foundation for later development.
It has been estimated that every minute in the life of a newborn baby, more than 4 million new nerve cells branches are created in the brain. This process does not happen by itself. The brain needs stimulation from the senses for branching and myelination to occur. Stimulation from the vestibular, tactile and kinaesthetic senses is especially important for this. The baby gets this stimulation by being touched and rocked by her parents and continually making rhythmic baby movements on her own. Such movements develop in a certain order according to an inborn programme which can have individual variations.
Turning around, creeping on the stomach, rocking and crawling on hands and knees are some important milestones in this development. The stimulation the brain receives from such rhythmical baby movements during the first year of life is fundamental for the future development and maturing of the brain.
When the nerve connections and synapses of the brain increase in number, additional parts of the brain start to perform their functions in new nerve patterns, which are stimulated by the infant’s movements. This is a process that continues automatically even when the nerve cells do not get direct stimulation. At the same time is a pruning of nerve connections corresponding to old behavioural patterns that the child no longer needs.
In children who have not had sufficient stimulation of this kind, the maturing of the brain is delayed or impaired. Such delayed development can appear as an attention disorder with or without hyperactivity.
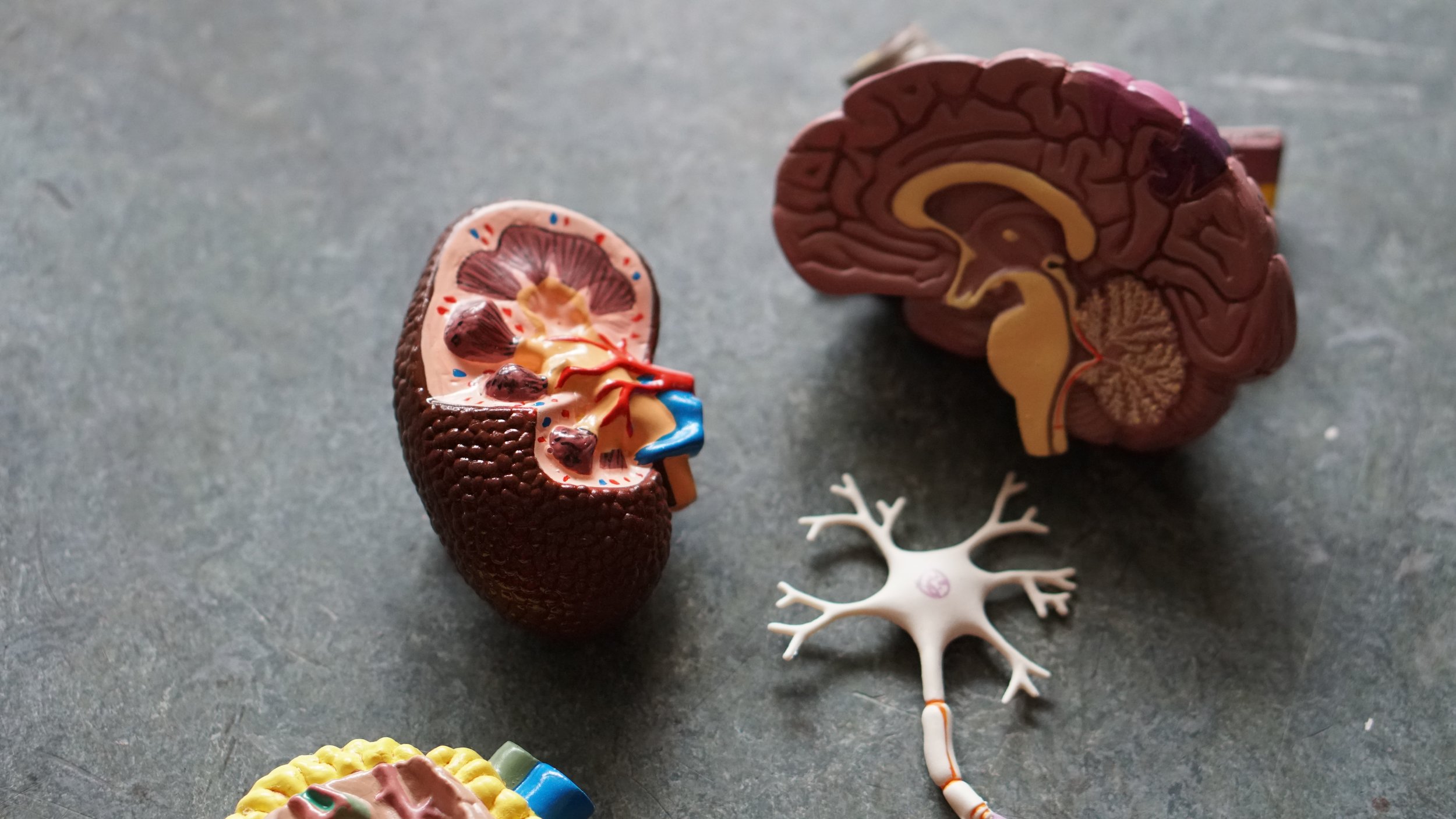
According to the American scientist Paul MacLean, who studied the development of brains in reptiles, mammals and humans, the human brain consists of three layers that cap the brain stem like the layers of an onion and work as guiding operators for the neural chassis. It is referred to as the triune brain.
The first layer is the reptilian brain which corresponds to the brain of reptiles. In humans the reptilian brain is called the basal ganglia, one task of which is to control our postural reflexes.The reptilian brain must also inhibit the primitive reflexes: which are inborn, stereotyped movement patterns controlled by the brain stem. The primitive reflexes constitute the movements of the foetus and the newborn infant. They must be transformed into the postural life-long reflex movement patterns in order for the child to be able to rise, walk and keep her balance. The basal ganglia also regulate the level of activity of the child and ensure that the child is not revved up most of the time.
The next layer is the mammalian brain, or the limbic system, that controls, among other things, our emotions, memory, learning and the ability to play. The outer layer is the neocortex. signals from the sense organs must reach the neocortex and be processed there in order for us to be aware of what happens around us and be able to act consciously. The prefrontal cortex is of crucial importance for our judgement, attention, and power of initiative and control of impulses.
When we are born, all parts of the brain have been established however not yet working well together. In order for all parts to function as a unit they must be developed and linked up to each other. This is achieved by rhythmic infant movements that stimulate the growth and branching off of the nerve cells and the myelination of the nerve fibres.
The infant needs to develop sufficient muscle tone in order to be able to move around and stimulate this linking together. To establish tone, the infant needs to be touched, hugged and rocked, as well as being allowed to move around freely. Such stimulation sends signals from the sense organs of the tactile, balance and kinaesthetic senses to those centres of the brain stem that regulate muscle tone. if the baby gets insufficient stimulation from these senses the tone of the extensor muscle will be low. This may make it difficult for the baby to lift her head and chest and move around, further reducing the stimulation from the balance, tactile and kinaesthetic senses, leading to a particularly vicious cycle of developmental delay.
When a baby is unable to move around freely, too little stimulation is conveyed to the neocortex via the Reticular Activation System (RAS) of the brain stem. The task of this system is to arouse the neocortex. When there is insufficient arousal, the child will become sluggish and inattentive to sensory signals. Moreover the nerve cells and the nerve nets of the neocortex will not develop properly.
The cerebellum is also important for the linking up of the brain and development of our ability to pay attention. One task of the cerebellum is to make our movements rhythmic, coordinated and smooth. From the cerebellum, there are important nerve connections up to the prefrontal cortex and the centres of speech in the frontal lobe of the left hemisphere.
At birth, the cerebellum is immature and it grows substantially after the age of 6 months. The rhythmic baby movements develop the nerve nets and nerve cells of the cerebellum and its connections to the frontal lobes. That is one reason why rhythmic movements are so important for the linking up of the frontal cortex and the development of the power of attention and speech.
The sensory stimulation caused by the rhythmic movements encourages the growth of the nerve nets of the brain stem, cerebellum, basal ganglia and neocortex to develop. This causes attention and concentration to improve and hyperactivity and impulsivity to decrease.
The rhythmic movements also increase the muscle tone of the extensor muscles that straighten the back and keep the head in an upright position. Body posture, breathing and endurance will improve and the neocortex will be aroused by stimulation via the brain stem, which improves attention and concentration.
The movements stimulate the cerebellum and its nerve pathways to the prefrontal cortex, which also improves attention and concentration and diminishes impulsivity. RMT also stimulates the basal ganglia to mature and integrate the primitive reflexes, which then facilitates the ability to regulate levels of activity and be still.
When the motor development of the infant is impeded in some way the maturation process of the brain may be impaired or delayed. The reasons can be many for such obstructed motor development: birth injury, microwaves, toxicity from heavy metals, genetic factors, cultural and psychological factors, etc. This delayed maturation of the brain may very well be the cause of the various challenges with motor function, attention, impulse control, learning, etc that many people have.


